Advanced Care Planning in ALS
Outline
- Introduction
- Epidemiology and Prognosis of ALS
- Diagnosis
- Diagnosis Communication
- Drug Treatment
- Disease Modifying
- Survival Prolongation
- Symptomatic Treatment
- Multidisciplinary Care
- Respiratory Care
- Nutrition
- Caregiver Fatigue
- End of Life Care
Introduction
What is ALS?
Epidemiology
- Median survival: 20-48 months from symptom onset
- Mean age of onset: 50 years old
- Incidence: 1.4 cases per 100,000
- M:F: 170:100
- Cumulative lifetime risk: 1:300 or 1:400
- Philippine Data: None
Diagnosis
- Evidence of LMN degeneration by clinical, neurophysiological and
neuropathologic means - Evidence of UMN degeneration by clinical means
- Progressive symptoms affecting a region or regions
- Absence of other disease that can explain the above symptoms
| Upper Motor Signs (Brain) | Lower Motor Signs (Brainstem and Spinal Cord) |
|---|---|
| • Spasticity | • Weakness |
| • Hyperreflexia | • Fasciculations |
| • Spreading reflexes | • Atrophy |
| • Pathologic Reflexes |
- El Escorial Criteria
- Revised El Escorial Criteria
- Awaji Criteria
| Segment | Muscles Involved | UMN | LMN |
|---|---|---|---|
| Bulbar | Facial muscles, Tongue, Muscles for speech and deglutition | Exaggerated gag, snout reflex, pseudobulbar affect and forced yawn | Atrophic tongue and facial muscles, Dysphonia, Dysphagia |
| Cervical | Muscles in the Upper Extremities | Hoffman, Tromner and finger flexor reflexes | Weakness, atrophy, fasciculations in the Upper Extremities |
| Thoracic | Muscles of respiration and paraspinal muscles | Loss of superficial abdominal reflexes | Respiratory problem |
| Lumbosacral | Lower extremities | Extensor plantar reflexes | Weakness, atrophy and fasciculations in the lower extremities |
Diagnosis
- Clinically Definite
- Clinically Probable
- Clinically Probable- Laboratory Supported
- Clinically Possible
Diagnosis
- Clinical signs with high sensitivity and specificity
- Split Hand Syndrome
- Split Hand Index
- Neuromuscular ultrasound in detecting fasciculation
- Clinically Probable- Laboratory Supported
- Axonal Excitability Studies
Disease Communication/Breaking the News in ALS
- Represents the beginning of treatment
- Basis of the patient’s autonomy
- The first things said are often the most remembered
Why breaking bad news is difficult for doctors?
- Fear of messenger being blamed for the bad news
- Perceived lack of time
- Lack of training
- Fear of being asked difficult questions causing distress
- Invoking fears of one’s own mortality
Process of Diagnosis Communication
- Quiet and comfortable location, convenient time, permitting the
patient to question or express doubts with the patients relatives or
caregivers present - Clear language
- Non verbal communication is important
Content of Diagnosis Communication
Preference:
- 87% prefers to have as much information as possible
- 5% prefers to have additional information only if it was optimistic
- 8% leave to the discretion of their physician
Content:
- 60% wants to know the disease (not the name)
- 54% wants to know about treatment and outcome
- 8% leave to the discretion of their physician
Drug Treatment
- Disease Modifying Drugs: None
- Survival Prolonging Drugs
• Riluzole: offers 2-3 months survival benefit which may be greater in those
with bulbar onset and younger patients
• Edaravone: decline on the ALS FR by 2.49 points fewer than placebo group
• Downside: stringent inclusion criteria, limited duration of data - Symptomatic Treatment
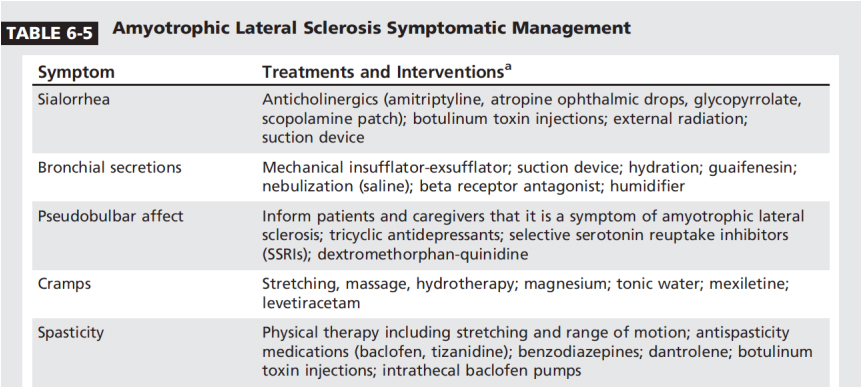
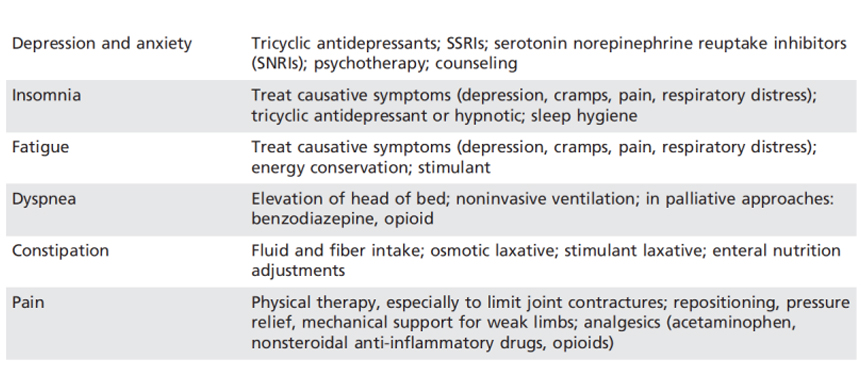
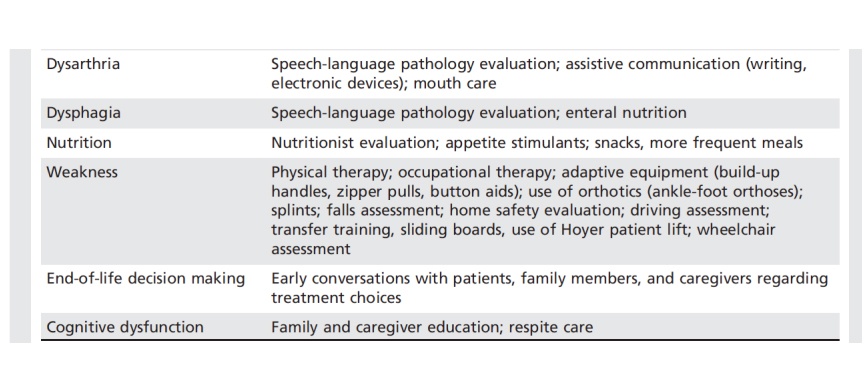
Symptomatic Treatment
Multidisciplinary Care
- Respiratory Care
- Nutrition
- Communication
- Caregiver Fatigue
Respiratory Car
Goals:
- Prolong survival
- Improve quality of life
Mechanism of respiratory failure in ALS:
-Loss pf phrenic nerve function
Signs and symptoms of respiratory failure
- Difficulty in speech
- Difficulty in airway clearance
- Aspiration as bulbar muscle coordination declines
Surrogates for respiratory function
- Forced Vital Capacity
- Maximum Inspiratory Pressure
- Maximum Expiratory Pressure
Guidelines for qualification of respiratory assist device
- Diagnosis of ALS plus
- O2 sats of <89% for 5 mins on overnight oximetry
- Increased PaCO2 of >45 mmHg or
- FVC <50%
- MIP < -60 cm H20
Respiratory Assistive Devices
- Non- Invasive Ventilation (NIV)
- Standard of care for respiratory support in patients with ALS
- Appropriate time to start: unclear but new data suggest that early NIV
adaption in the disease course (FVC >80%) may provide additional mortality
benefit
- Diaphragmatic Pacing
- Not recommended
- Mechanical Insufflation- Exsufflation
- Augment respiratory mechanics and produce an adequate cough
- Tracheostomy
- Only 2-5% undergo tracheostomy
- In theory, best done prior to emergent/urgent need but in reality, often occur in times of acute respiratory failure
- Patients who choose tracheostomy:
- Younger
- Have young children
- Higher degrees of education
- High socio economic status
- Definitely not doctors ?
Nutrition
- Dysphagia and aspiration
- Malnutrition
- Severe weight loss
- Dehydration
- Aspiration pneumonia
PEG
- No firm rules regarding the timing of feeding tube
AAN Guidelines: should be offered at the onset of symptomatic
dysphagia and accelerated weight loss:
- Preferably done prior t significant respiratory functional decline (FVC<50%)
- PEG may still be offered in patients with declining respiratory function
*No studies: oral vs enteral feeding
Nutrition
- High calorie and protein enriched diets combined with snacks and nutritional shakes are encouraged
Communication
- Successful communication strategies can improve quality of life especially as some patients with ALS will lose effective verbal communication
- Options:
- Writing (Pen and Paper) or E-writers
- Text to speech applications
- Eye gaze technologies
- Voice banking options
- One push solution for medical emergencies
End of Life Care
- Conversations regarding end of life decision-making should be held early in the disease course before a respiratory or nutritional crisis occurs
- Quality of life discussions include defining what interventions are consistent with the patient’s wishes
- Palliative and hospice care may have a role
- Caregiver fatigue and burden should be assessed on a ongoing basis
