Advanced Care Planning in Amyotrophic Lateral Sclerosis
Mario B. Prado Jr., MD, FPNA
Outline
- Introduction
- Epidemiology
- Diagnostic Criteria
- Diagnosis Communication/Breaking the Bad News
- Treatment
- Respiratory Care
- Nutrition
- End of Life Care
- Opportunity for Research
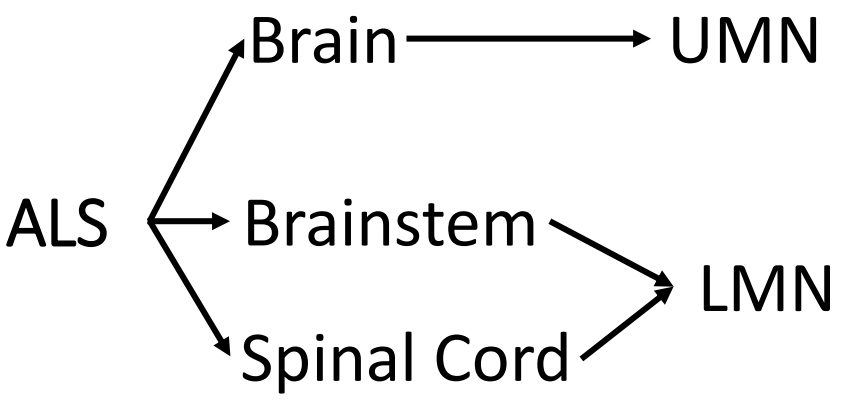
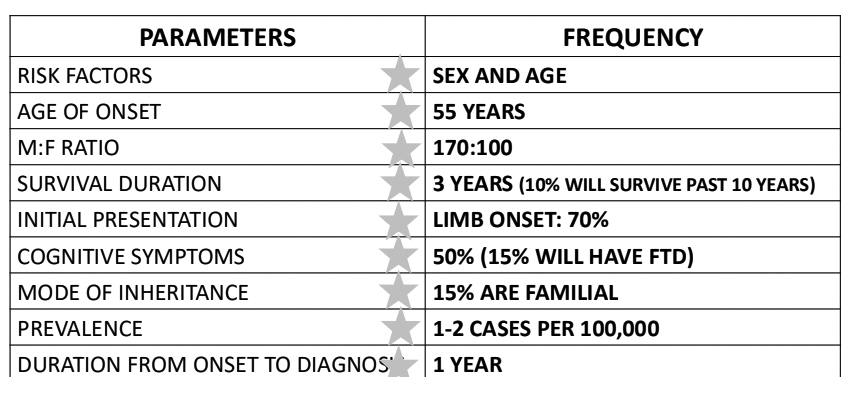
Epidemiology
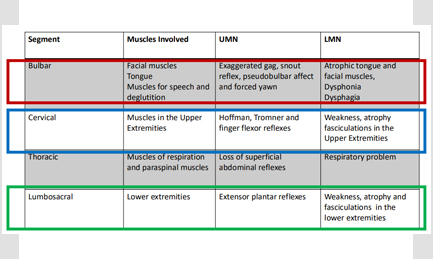
Diagnosis
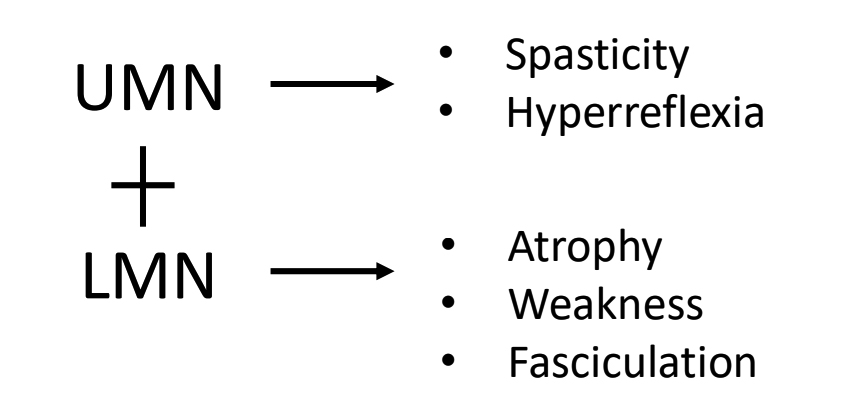
PSEUDOBULBAR PALSY, FORCED YAWN, JAW AND SNOUT REFLEXES
TROMNER, HOFFMAN, FINGER FLEXOR REFLEXES
ABSENT ABDOMINAL REFLEX
BABINSKI SIGN
- ACTIVE DENERVATION: FIBRILLATION AND PSW
- RE-INNERVATION: HIGH AMPLITUDE POLYPHASIC MUP’s
EL ESCORIAL, MADRID, SPAIN

AWAJI, HYOGO PREFECTURE, JAPAN

Revised El-Escorial Criteria
- BULBAR REGION
- DEFINITE ALS: 3 SEGMENTS
- CERVICAL REGION
- PROBABLE ALS: 2 SEGMENTS
- THORACIC REGION
- LABORATORY SUPPORTED: 1 SEGMENT +2 LMN DIAGNOSED BY EMG NCS
- LUMBOSACRAL REGION
- POSSIBLE ALS
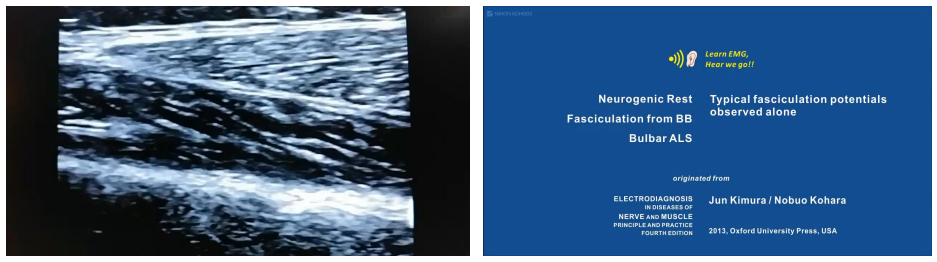
El Escorial Criteria vs Awaji Criteria
- Awaji recognizes the importance of electrophysiologic findings in the diagnosis of ALS (Active Denervation with Reinnervation)
- Electrophysiologic findings may be found before overt weakness appear
- Electrophysiologic findings have the same weight as LMN clinical signs
- Probable ALS- Laboratory Supported removed
- Specificity: 99.5%
- Sensitivity: 45→57%
ACTIVE DENERVATION: FIBRILLATION AND PSW RE-INNERVATION: HIGH AMPLITUDE POLYPHASIC MUP’s
Gold Coast Criteria
- .Progressive motor impairment – documented by history or repeated clinical
assessment, preceded by normal motor function,
and - .Presence of upper and lowers motor neuron dysfunction in at least 1 body region, (with upper and lower motor neuron dysfunction noted in the same body region if only one body region is involved) or lower motor neuron dysfunction in at least 2 body regions, and
- Investigations excluding other disease processes

New Ancillary Methods
- Neuromuscular Ultrasound
- Non invasive way of detecting fasciculations in patients with ALS
- Done by placing the probe in the affected muscles including the tongue
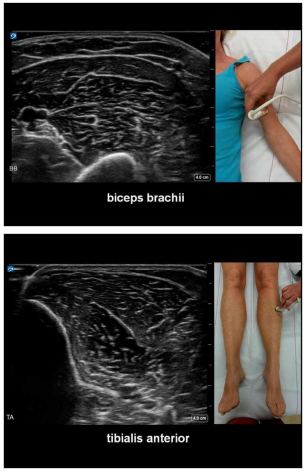
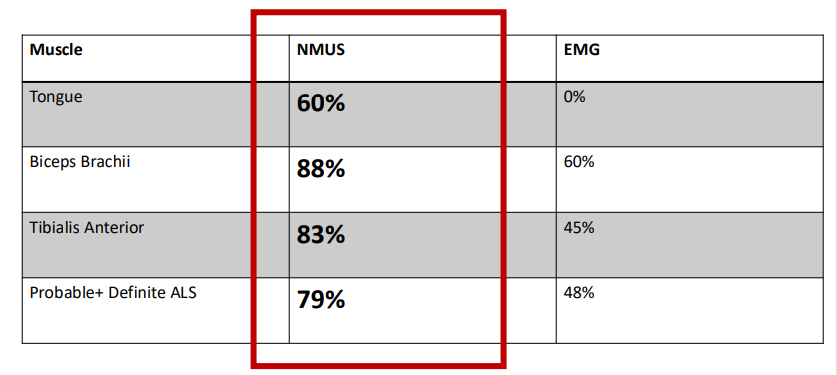
Sensitivity of NMUS vs EMG in detection of
fasciculation in select muscles of patients with ALS
Excitability Studies
- Threshold Tracking Transcranial Magnetic Stimulation – decreased cortical inhibition = hyperexcitable upper motor neurons
- Axonal Excitability Studies – increased axonal membrane depolarization= shyperexcitable lower motor neurons

Dissociated muscle atrophy
- SPLIT HAND SIGN
- SPLIT ELBOW SIGN
- DISSOCIATED LEG MUSCLES
DIAGNOSIS COMMUNICATION
BREAKING THE BAD NEWS
Why breaking the bad news is difficult for
doctors?
-
- Fear of messenger being blamed for the bad news
- Perceived lack of time
- Lack of training
- Fear of causing distress
- Fear of being asked difficult questions
- Invoking fears of one’s own mortality
Diagnosis Communication
- Marks the end of the diagnostic process and represents the start of treatment
- 82% of doctors in US and Europe deliver the
news right away - 20% of patients are told about their
diagnosis in Japan
Beneficence vs Autonomy
Diagnosis Communication
Process
- In person
- In a quiet and comfortable location
- At a convenient time
- Permitting the patient to question or express doubts
- Patient should be accompanied by caregiver
Content
- Course and outcome (74%)
- Disease modifying therapies (68%)
- Ongoing research (68%)
- Specific name of illness (11%)
- Pharmacology (8%)
Multidisciplinary Approach
- Neurologist
- Pulmonologist
- Respiratory Therapist
- Rehabilitation MD
- Occupational Therapist
- Physical Therapist
- Gastroenterologist
- Nutritionist
- Palliative Care Physician
- Etc
Is There a Cure?
Riluzole
- Anti-glutamate drug
- Dose: 100mg daily
- Improve the 1 year survival by 15%
- Prolong survival by 3 months after 18 months of intake
- NNT: 11
- More benefit: 1)Younger patients with bulbar onset 2) longer diagnostic delay
- NOT AVAILABLE IN THE PHILIPPINES
Other drugs
- Edaravone
- Free radical scavenger
- Use is limited by:
- stringent inclusion criteria
- Limited duration of data
- Complicated mode of administration
- High Dose Vitamin B
- Not yet published
No cure for ALS until now
Symptomatic Management
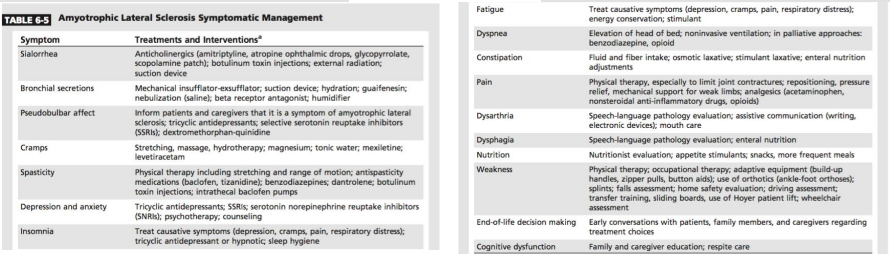
- Sialorrhea- amitriptyline, scopolamine, glycopyrrolate, atropine drops, BOTOX injection, irradiation
- Spasticity- regular physical therapy, baclofen, tizanidine
- Cramping- levetiracetam, mexiletine
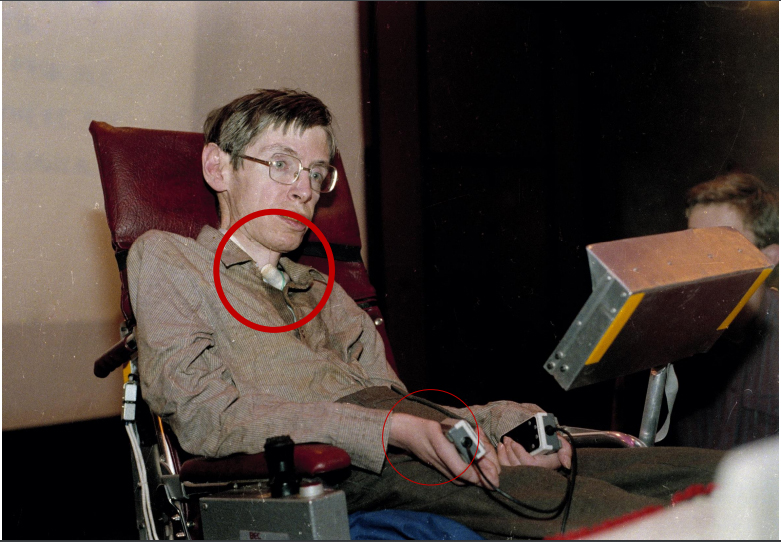
- Dysarthria/Communication
- Writing (pen and paper) or E-writers
- Text to speech applications
- Eye Gaze technologies
- Voice banking options
Respiratory Care
- Due to degeneration of the phrenic nerve
- Initial manifestations:
- Nocturnal hypoventilation
- Morning headaches
- Orthopnea
- Easy fatigability
- Indications for Respiratory Assistive Device (NIV and IMV)
- Dyspnea
- O2 saturation is below 89%
- CO2 is above 45 mmHg
- FVC is below 50%
- SNIP is below 40%
- MIP is above 60 cm H2O
- NON INVASIVE VENTILATION
- Improves quality of life and survival by at least 1 year
- Part of standard of care for patients with ALS
- INVASIVE MECHANICAL VENTILATION
- If no improvement after NIV has been maxed
- Improve QOL and survival for at least 2 years
- Only 5% want tracheostomy
Other Respiratory Care Concerns
- Mechanical Insufflation- Exsufflation- 3-5 coughs done in rapid succession several times a day
- Diaphragmatic Pacing (DP)- more mortality among patients in DP were observed hence this technique is currently not recommended.

Nutrition
- 5% weight loss= 30% increased risk of death
- Recommendations:
- Adequate calorie diet
- Dietary texture modification
- Use of adaptive eating utensils
- Use of swallowing techniques (supraglottic swallow and chin tuck maneuver)
When do we advise PEG insertion?
- Weight loss of around 5-10%
- BMI of less than 20mg/kg
- Presence of bulbar symptoms
- FVC of more than 50%
- PRG is recommended if FVC is less than 50%
- Parenteral nutrition is recommended if PEG, PRG or NGT is contraindicated
End of Life Care
- Hospice Care (Non-malignant admissions)
- 48% ALS
- 18% Pulmonary (COPD)
- 13% Cardiovascular (Heart Failure)
- 10% Neurologic (Stroke)
- 10% Other Diagnosis
- Most common symptoms
- Dyspnea, Pain and Fatigue
- Dyspnea, Pain and Fatigue
- Difficult to swallow (87%)
- Receive antidepressant, antibiotics and laxatives
- Hospice Referral:
- Nutritional
- Functional
- Respiratory
- Conversations regarding end of life decision-making should be held early in the disease course before a respiratory or nutritional crisis occurs
- Quality of life discussions include defining what interventions are consistent with the patient’s wishes
- Palliative and hospice care may have a role
- Caregiver fatigue and burden should be assessed on a ongoing basis
Goals for the future
- ALS Referral Center
- Establishment of Prevalence and Incidence
- ALS support group
- Increase ALS research output
